'No Surprises Act' in effect; Contact 6 helps resolve medical bill

'No Surprises Act' in effect; Contact 6 helps resolve medical bill
Surprise medical bills can cost patients hundreds, even thousands of dollars. For years, Contact 6 has taken these billing complaints to insurance companies. But now, there should be a drop-off in those cases.
MILWAUKEE - Surprise medical bills can cost patients hundreds, even thousands of dollars. For years, Contact 6 has taken these billing complaints to insurance companies. But now, there should be a drop-off in those cases.
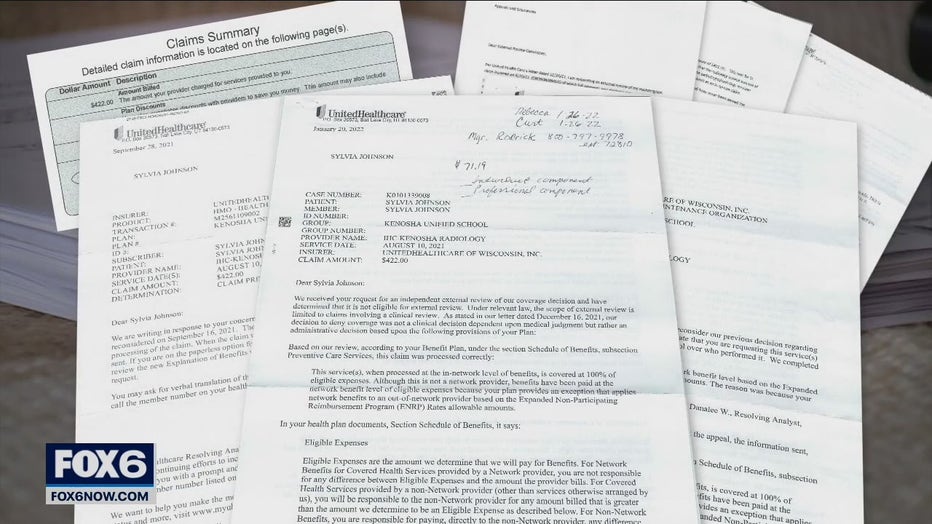
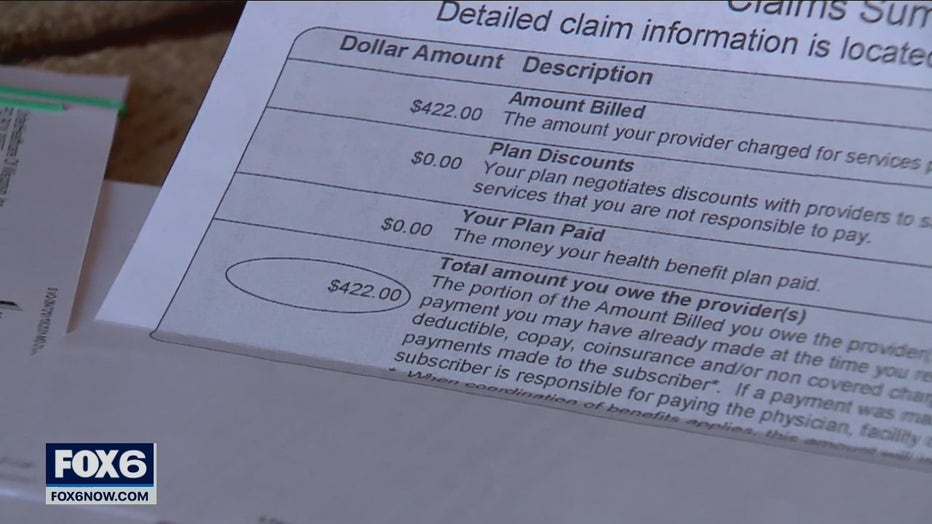
On Sylvia Johnson’s kitchen table is a pile of documents. It’s the fall-out from her annual wellness visit back in August. In Sylvia’s file is her surprise medical bill, records from her three repeals to insurance, and her three rejections for full-coverage.
"[The appointment has] always has been covered which was so odd," said Johnson.
Johnson says she’s had the same appointment every year for about twenty years. This time, she got a bill for $422 dollars.

SIGN UP TODAY: Get daily headlines, breaking news emails from FOX6 News
"The radiologist portion was out-of-network and not covered," said Johnson.
Johnson discovered that even though her hospital was in-network with her insurer, the radiologist who read her mammogram was not. It’s a person Johnson never met and never thought to ask about.
"[The insurer] made it sound like the member was the responsible person," said Johnson.
Medical billing is consistently a top ten consumer complaint in Wisconsin, according to the Department of Agriculture, Trade and Consumer Protection. Were Johnson to have the same appointment today, she’d likely never see the bill.
On January 1st, 2022, the No Surprises Act went into effect. It provides broad consumer protections against surprise medical bills.
Wisconsin Commissioner of Insurance Nathan Houdek says the new law safeguards millions of Americans and closes long-standing loopholes.
FREE DOWNLOAD: Get breaking news alerts in the FOX6 News app for iOS or Android
As of Jan. 1, the no surprises act provides broad consumer protections against surprise medical bills.
"When they’re in a situation where they unknowingly receive care from an out-of-network provider," said Houdek.
Under the No Surprises Act, the patient still pays co-pays and deductibles but cannot be asked for pay more for out-of-network care at an in-network facility for emergency medicine, anesthesiology, radiology or lab services.
Patients can agree in advance to be treated by an out-of-network provider, in some cases, like choosing a specific surgeon knowing the cost will be higher.
"When I saw that, I thought that’s exactly my situation," said Johnson, of the No Surprises Act.

Johnson’s bill was lowered to $355 by UnitedHealthcare before she wrote to Contact 6. The FOX6 consumer segment wrote to the hospital and insurer on her behalf. Soon after, both said the bill was dropped.
UnitedHealthcare tells Contact 6:
"We reached out to the physician’s office who agreed to waive this 2021 out-of-network radiology bill. The ‘No Surprises Act,’ which went into effect beginning Jan. 1, 2022, prohibits care providers from sending surprises bills in cases like this where the patient received care from an out-of-network doctor at an in-network facility.
Froedtert South sent the following after conducting an internal review:
"Froedtert South contracts Radiology services through Envision Healthcare that was not a participating provider network of Radiology with UnitedHealthcare as of January 1, 202. Unfortunately, from a global perspective, network providers in various specialty areas are not always updated with respect to in-network inclusion or exclusion. The invoice received by the patient would not have come from Froedtert South…
The patient contacted Envision Healthcare, presumably after receiving her patient responsibility invoice (s) after several direct appeals to UnitedHealthcare and Envision Healthcare adjusted their "amount due" to $0.00. Very admirable on their behalf since the patient should not be penalized for a network error."
The No Surprises Act only applies to medical bills sent after January 1, 2022. Patients on Medicare and Medicaid already had these protections in place.
Featured
Matthew Willmann sentenced, pay fines in off-duty incident as officer
A Milwaukee County judge sentenced Matthew Willmann to pay $1,250 in fines (the maximum allowed) and $1,099 in restitution to UW-Milwaukee. Willmann is a Milwaukee police officer who was involved in an incident that happened in July 2020 while he was off-duty.
Featured
Milwaukee host RNC? Politico report says city leads competition
A report by Politico indicates Milwaukee leads the competition to host the 2024 Republican National Convention.
Featured
Menomonee Falls Aldi theft, 2 suspects sought
The Menomonee Falls Police Department is investigating a retail theft that occurred at Aldi on Leon Road on Jan. 30.




