FOX6 Investigators take you inside a COVID-19 ICU amid pandemic

FOX6 Investigators take you inside a COVID-19 ICU amid pandemic
Wisconsin's fall COVID-19 surge is testing the state's 134 hospitals. One of them invited us inside the ICU.
MADISON, Wis. - Wisconsin's COVID-19 surge this fall is testing the limits of the state's 134 hospitals. One of them invited the FOX6 Investigators to see what it's like in the COVID-19 intensive care unit.
At the University of Wisconsin Hospital in Madison, a brand new, state-of-the-art hospital wing was ready to be opened for patients undergoing brain surgery. Then came the pandemic. Now, the 4th-floor wing has been converted to an expanded COVID-19 intensive care unit where the patients are so sick they cannot breathe on their own.
COVID-19 ICU at UW Hospital in Madison
“We use medications to paralyze every muscle in the patient’s body so the ventilator can take over complete control," said Janielle Raven, an ICU nurse.
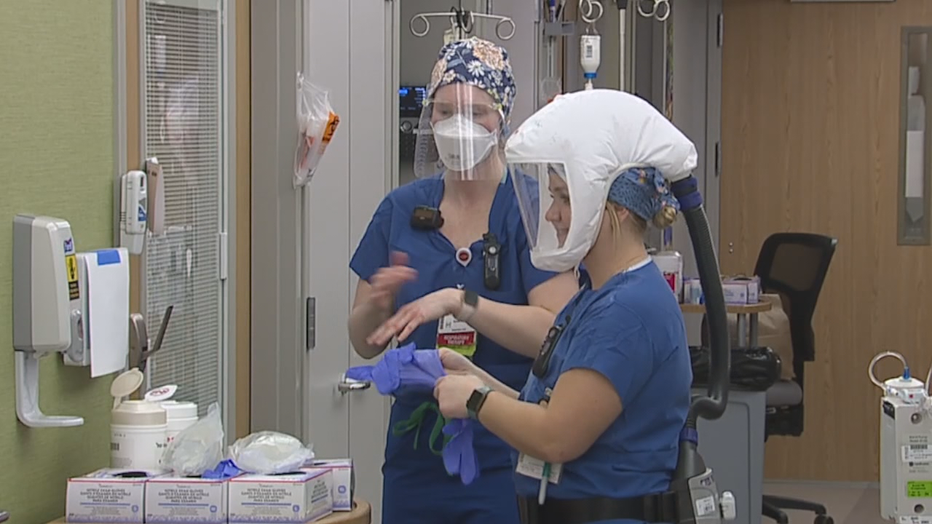
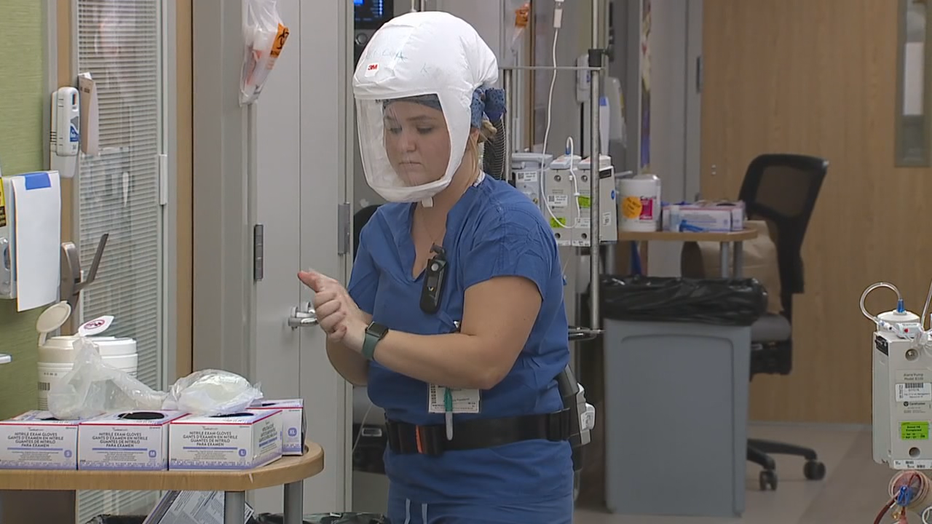
No matter how much protective gear they put on, the critical care workers in this unit are not immune to fear.
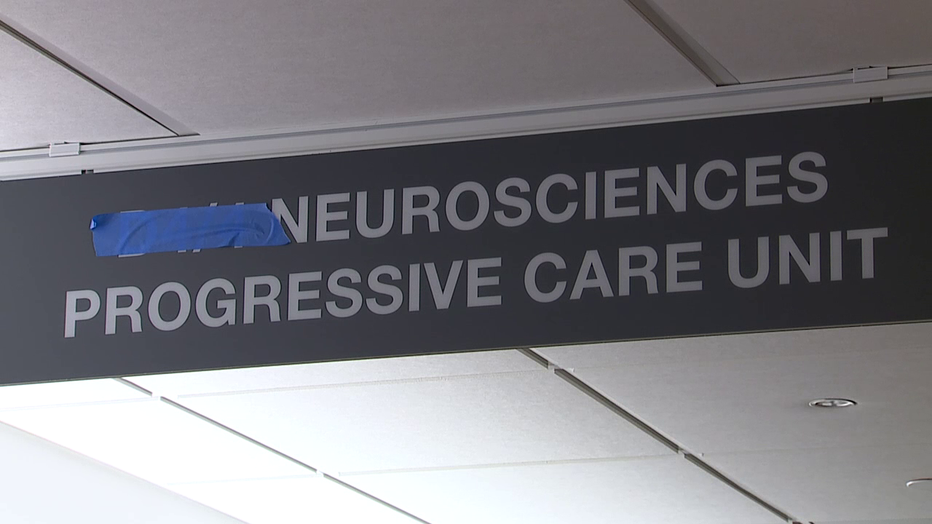
UW Health recently converted a brand new wing built for brain surgery patients into a COVID-19 intensive care unit.
“We are right in the face of COVID," said Samie Linscheid, a respiratory therapist who is often situated at the head of a bed occupied by a COVID-19 positive patient. “It is very dangerous and it is scary.”
“When we first started taking care of COVID patients, my wife didn’t want me to come home," said Dr. Scott Wilson, a hospitalist at UW Health who's been treating COVID-19 patients since the beginning of the pandemic.
Still, day after day, they go to battle with a deadly, airborne virus.
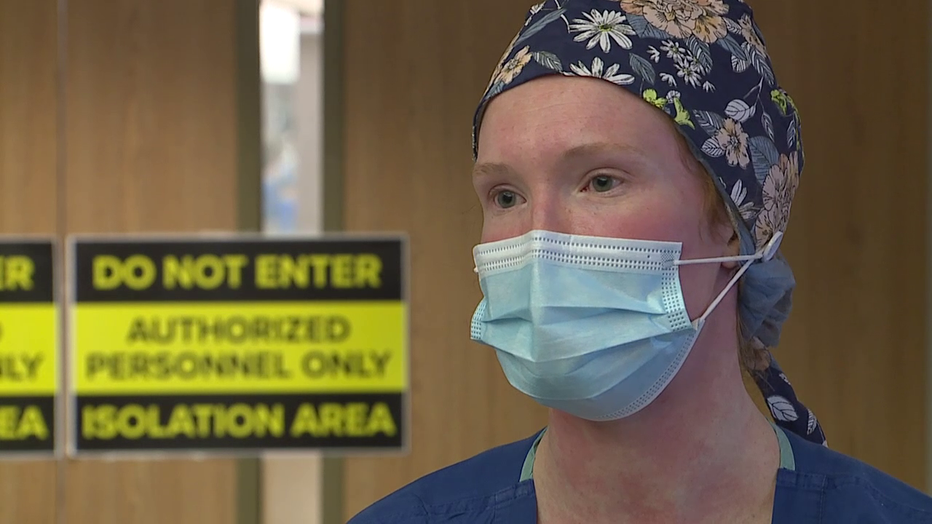
“It’s nothing that I’ve ever seen in my 15 years as a nurse," Raven said.
COVID-19 ICU at UW Hospital in Madison
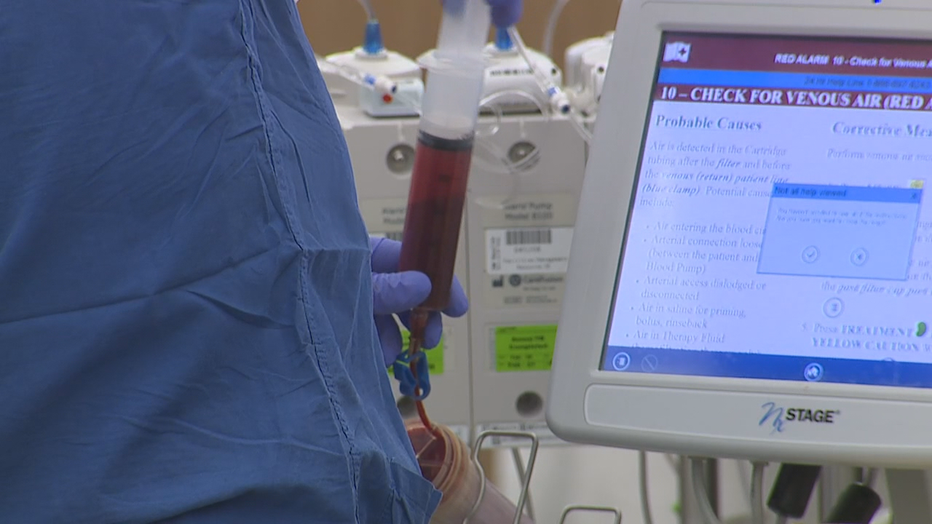
To keep patient contacts to a minimum, equipment that is usually found inside a hospital room is instead outside the room, with cables and tubes strung through holes in the wall.
“Patients on ventilators have their controls sometimes outside the room," Dr. Wilson said. "Their IV poles may be outside the room."
And family members are not allowed to visit.
“Very strange," said Dr. Wilson. "It’s really difficult for patients.”
That means doctors and nurses in full protective gear may be a dying patient's only human contact.
Samie Linscheid, first-year respiratory therapist
“You have a mask on," Linscheid said. "They can’t understand what you’re saying half the time, because they can’t read your lips.”
In her first year as a respiratory therapist, Linscheid admits she was underwhelmed when the pandemic first hit last spring.
“I was like, 'We don’t have that many COVID patients. It's not that bad.'"
“And then we had a decent summer," Raven said.
But all of that changed this fall.
“It’s just been totally off the wall.”
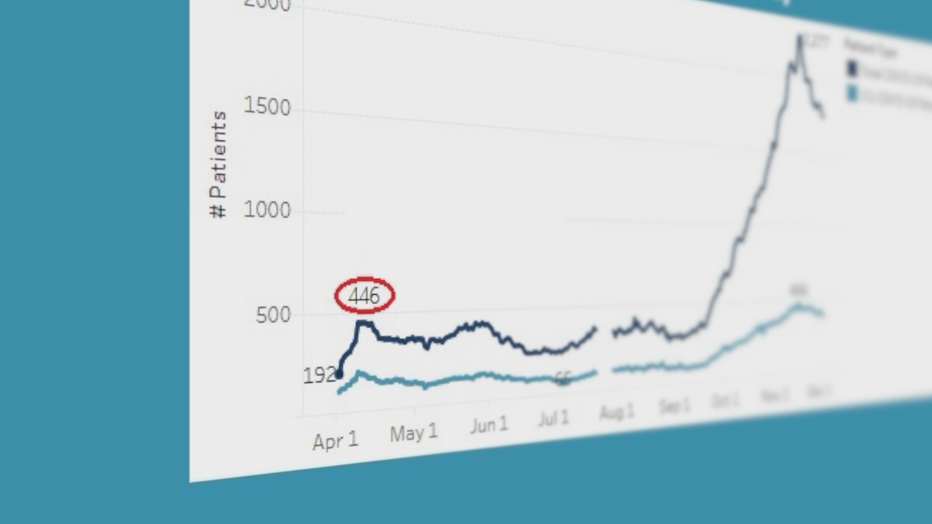
Even at the peak of the first wave in April, there were never more than 446 COVID-19 patients hospitalized all across the state.
It’s hard for me to understand," Linscheid recalls thinking. "Yes I want to follow these guidelines, but the hospital’s not horrible."
COVID-19 ICU at UW Hospital in Madison
In November 17th, there were more than 2,200 COVID-19 patients.
"Now, it is horrible," Linscheid said.
In the past few weeks, hospitalizations have dropped by more than 600. But there are still nearly four times as many COVID-19 patients now as there were last spring.
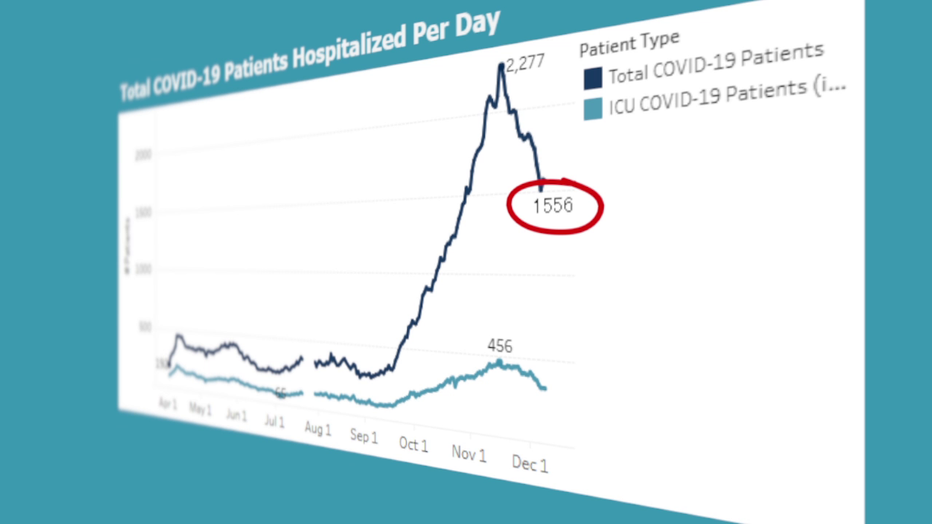
Even after a recent drop, the number of hospitalized COVID-19 patients statewide is still nearly 4 times the peak from last spring.
“Eleven wings in our hospital right now have been converted to COVID wings," said Dr. Jeffrey Pothof, Chief Quality Officer for UW Health. However, he says, it's not just rooms that are in short supply. Health care workers are running on fumes.
“We can’t create more staff and particularly critical care staff," Raven said.
“I don’t have a magic button or magic wand that creates more critical care doctors, critical care nurses, respiratory therapists," Dr. Pothof said.
"It's exhausting," said Linscheid. "Being in the ICU, the vents are constantly alarming, patients are constantly decreasing their oxygen.”

UW Hospital in Madison
And yet, exhaustion is not the worst part.
“The toughest moments for me are always the moments before the patient goes on life support," Raven said.
“It takes a lot out of you," Linscheid added.
"I’m doing a lot of hand-holding, reassuring, drying tears. I’ve prayed," Raven said, her voice catching as she choked up, then sighed. "Those are the tough ones.”
In the final month of 2020, there are signs of hope. Positive cases are down. Hospitalizations are dropping. And, perhaps most importantly...
“The vaccines are coming," said Dr. Pothof.
FREE DOWNLOAD: Get breaking news alerts in the FOX6 News app for iOS or Android
But there is still fear.
"I’m worried we’re going to see more and more of this as we go through the winter," Raven said.
“If we were to see another huge surge because of Thanksgiving, that could overrun us in the next couple of weeks. If we don’t see that surge, we could make it ‘til Christmas.”
In other words, it's too soon for Wisconsin to breathe easy.
UW Health says COVID-19 patients are filling about 12 to 18 percent of their in-patient beds. That's somewhere between 1-in-5 or 1-in-6 patients. The rest of the beds are still devoted to those battling things like cancer, strokees, burns, and heart attacks.

Wisconsin vaccine committee recommends EMS in top tier for shots
Sometimes they put out fires, but far more often, Wisconsin firefighters are responding to medical calls.
Featured
DHS campaign aims to boost flu vaccine rates in communities of color
Wisconsin’s Department of Health Services (DHS) launched on Wednesday, Dec. 9 the “Be an InFLUencer” education and awareness campaign.
Featured
COVID-19 testing down in Wisconsin; residents await vaccine
Officials say the average number of test kits administered per day is down 10,000 compared to two weeks ago.



